What Is Painful Heel And Techniques To Overcome It
Overview
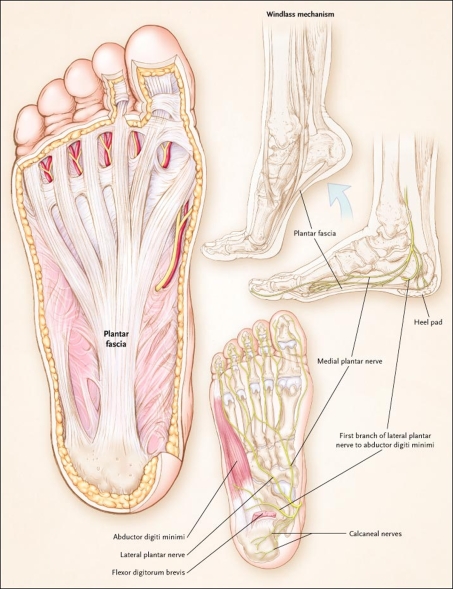
Plantar fasciitis is a painful condition affecting the connective tissue that stretches between the heel and the middle of the foot. It is usually caused by overuse, injury or muscular abnormalities. In extracorporeal shockwave therapy, a machine is used to deliver sound waves to the painful area. It is not known exactly how it works, but it is thought that it might stimulate healing of the fascia.
Causes
Plantar fasciitis is common in sports which involve running, dancing or jumping. Runners who overpronate where their feet roll in or flatten too much are particularly at risk the plantar fascia is over stretched as the foot flattens. A common factor is tight calf muscles which lead to a prolonged or high velocity pronation or rolling in of the foot. This in turn produces repetitive over-stretching of the plantar fascia leading to possible inflammation and thickening of the tendon. As the fascia thickens it looses flexibility and strength. Other causes include either a low arch called pes planus or a very high arched foot known as pes cavus. Assessing the foot for plantar fasciitisExcessive walking in footwear which does not provide adequate arch support has been attributed. Footwear for plantar fasciitis should be flat, lace-up and with good arch support and cushioning. Overweight individuals are more at risk of developing plantar fasciitis due to the excess weight impacting on the foot.
Symptoms
Plantar fasciitis has a few possible symptoms. The symptoms can occur suddenly or gradually. Not all of the symptoms must be present at once. The classic symptom of plantar fasciitis is pain around the heel with the first few steps out of bed or after resting for a considerable period of time. This pain fades away a few minutes after the feet warm up. This symptom is so common that it symbols the plantar fasciitis disorder. If you have it then probably you have plantar fasciitis. If you don’t suffer from morning pain then you might want to reconsider your diagnosis. Pain below the heel bone at the connection of the bone to the fascia. As the condition becomes more severe the pain can get more intense during the day without rest. Plantar fasciitis symptoms include pain while touching the inside of the heel or along the arch. Foot pain after you spend long periods of time standing on your feet. Pain when stretching the plantar fascia. Foot pain that worsens when climbing stairs or standing on the toes. Pain that feels as though you are walking on glass. Pain when you start to exercise that gets better as you warm up but returns after you stop.
Diagnosis
Your doctor can usually diagnose plantar fasciitis just by talking to you and examining your feet. Rarely, tests are needed if the diagnosis is uncertain or to rule out other possible causes of heel pain. These can include X-rays of the heel or an ultrasound scan of the fascia. An ultrasound scan usually shows thickening and swelling of the fascia in plantar fasciitis.
Non Surgical Treatment
Many cases of plantar fasciitis can be treated with simple, conservative measures. These include ice packs, stretching exercises, anti-inflammatory medications, orthotic devices (custom molded orthotics), and physical therapy. It’s important to consult your doctor before you take any medications to treat this condition. In chronic or persistent cases, one of three techniques may be used to treat plantar fasciitis. Extracorporeal Shock Wave Treatment (ESWT). TOPAZ treatment. Platelet Rich P
lasma therapy.
Surgical Treatment
When more-conservative measures aren't working, your doctor might recommend steroid shots. Injecting a type of steroid medication into the tender area can provide temporary pain relief. Multiple injections aren't recommended because they can weaken your plantar fascia and possibly cause it to rupture, as well as shrink the fat pad covering your heel bone. Extracorporeal shock wave therapy. In this procedure, sound waves are directed at the area of heel pain to stimulate healing. It's usually used for chronic plantar fasciitis that hasn't responded to more-conservative treatments. This procedure may cause bruises, swelling, pain, numbness or tingling and has not been shown to be consistently effective. Surgery. Few people need surgery to detach the plantar fascia from the heel bone. It's generally an option only when the pain is severe and all else fails. Side effects include a weakening of the arch in your foot.
What May Cause Plantar Fasciitis To Surface
Overview
If you experience sharp, throbbing or aching heel pain with your first steps out of bed each morning, or when walking throughout the day, you may be suffering from Plantar Fasciitis. This guide will help you to understand the definition, symptoms and causes of this condition and will explore your treatment options for rapid relief from your pain.
Causes
Currently no single factor has been reliably identified as contributing to the development of plantar fasciitis. The two risk factors with the most support from current research. Decreased ankle dorsiflexion. Increased Body Mass Index (BMI) in non-athletic populations. These factors are related in that both lead to increased strain on the arch, both lead to increased compression on the heel. When dorsiflexion range of motion (ankle flexibility) is lacking, the body compensates by increasing movement of the arch. In this way, decreased ankle dorsiflexion influences pronation and places strain on the underside of the foot. Similarly, having a high BMI causes strain because it places a load on the foot that may be in excess of what the foot can support. As mentioned earlier, overpronation is thought to be a contributing factor, but studies on this have so far produced mixed results. The second way these factors relate to each other is in the way people stand. A lack of ankle flexibility and a high BMI can both cause increased pressure on the heel in standing. Keeping weight on the heels causes compression under the heel. But it also means the muscles and ligaments in the arch are not being used to balance your body weight. Lack of use, I suspect, is a greater danger than overuse. Looking beyond these potential contributors to heel pain though, there is one major factor that overshadows them all-the way footwear alters the normal function of the foot.
Symptoms
The classic sign of plantar fasciitis is that the worst pain occurs with the first few steps in the morning, but not every patient will have this symptom. Patients often notice pain at the beginning of activity that lessens or resolves as they warm up. The pain may also occur with prolonged standing and is sometimes accompanied by stiffness. In more severe cases, the pain will also worsen toward the end of the day.
Diagnosis
Your doctor can usually diagnose plantar fasciitis just by talking to you and examining your feet. Rarely, tests are needed if the diagnosis is uncertain or to rule out other possible causes of heel pain. These can include X-rays of the heel or an ultrasound scan of the fascia. An ultrasound scan usually shows thickening and swelling of the fascia in plantar fasciitis.
Non Surgical Treatment
You may experience concern in reading about treatment options for this condition that involve taking medications, having injections or undergoing surgery. While these remedies may be necessary in some cases, there are natural, non-invasive, affordable methods for treating and healing Plantar Fasciitis. A simple, three-step approach may be all you need to experience immediate or rapid symptom relief. Step 1) Give Your Feet A Rest. When a ligament is stressed and inflamed, it is absolutely essential to take pressure off it and let it rest. Adjust your daily habits to spend some time each day off your feet. Step 2) Ice Brings Cooling Relief. Apply an ice bag or cold pack to your heel for twenty minutes, twice a day. This will numb soreness and help control inflammation. Step 3) Gain Support From Orthotics. Orthotics are devices designed to modify body motions or lessen pressure on areas of the body. In the case of foot orthotics, these products may include splints, wraps and shoe inserts.

Surgical Treatment
Surgery may be considered in very difficult cases. Surgery is usually only advised if your pain has not eased after 12 months despite other treatments. The operation involves separating your plantar fascia from where it connects to the bone; this is called a plantar fascia release. It may also involve removal of a spur on the calcaneum if one is present. Surgery is not always successful. It can cause complications in some people so it should be considered as a last resort. Complications may include infection, increased pain, injury to nearby nerves, or rupture of the plantar fascia.
Prevention
Making sure your ankle, Achilles tendon, and calf muscles are flexible can help prevent plantar fasciitis. Stretch your plantar fascia in the morning before you get out of bed. Doing activities in moderation can also help.
Symptoms Of Heel Bone Spurs
If changing your shoes isn't helping to solve your foot pain, it is time for us to step in. Contact Dr. Jeff Bowman at Houston Foot Specialists for treatment that will keep your feet feeling great. Inserting arch support insoles in the shoes is also a good option.
Those affected by inflammatory conditions such as rheumatoid arthritis and Achilles tendonitis are also likely to experience pain and swelling in the ankles. If the joints in the feet get affected by osteoarthritis, it gives rise to pain, stiffness, swelling in or around the joint, and restricted range of motion. Since pain in the feet could be caused due to a variety of reasons, the treatment will depend on the underlying cause. Many a time, pain could be experienced by people who perform high-impact exercises such as running, jogging and other sports. Those who have been experiencing pain while running must make sure that they wear a good quality footwear. Painkillers or steroids might be prescribed for the treatment of a sprained ankle.

Another solution is to wear custom foot orthotics, like ezWalker ® Performance Custom Orthotics, in your shoes to help correct your body posture, stabilize your balance, relieve pain during follow-through and evenly redistribute your weight on your feet. EzWalker® Custom Orthotics are specifically made for each of your feet to properly support your arches while reducing pressure on the balls of your feet. With ezWalker® Custom Orthotics, you'll walk from lateral heel to medial forefoot for better biomechanics of your entire body. This condition manifests as a skin lesion that assumes a ring-like pattern. It can affect any region of the body, right from the scalp to the foot. One such common home remedy is the use of bleach. Many people claim that this is a very effective ringworm treatment.

Junctional Epidermolysis Bullosa: A condition that causes blistering of the skin because of a mutation of a gene which in normal conditions helps in the formation of thread-like fibers that are anchoring filaments, which fix the epidermis to the basement membrane. Kanner Syndrome: Also referred to as Autism, this is one of the neuropsychiatric conditions typified by deficiencies in communication and social interaction, and abnormally repetitive behavior. Kaposi's Sarcoma: A kind of malignancy of the skin that usually afflicts the elderly, or those who have problems in their immune system, like AIDS. For example, a year of perfect health is regarded as equivalent to 1.0 QALY.
Foot Problems Are Genetic
Podiatrists treat bunions, hammertoes, and all sources of toe and forefoot pain more than any other condition, save for heal pain and nail disease. There can be many complex mechanical causes for these conditions, as genetics has only an initial role in most cases of bunions and other toe and foot deformities. These conditions are successfully treated all day long by podiatrists, and should be the obvious first choice in care when foot pain develops. Sprains are a common injury, and often occur in the evenings or weekends after most medical practices are closed. It is very appropriate to present to an urgent care center or emergency room for serious foot and ankle sprains to ensure there is no fracture. These products can burn your skin.
Skin conditions that involve open sores, lesions, or contagions may also be treated with medical ointments and bandages or wraps. Skin disorders that are temporary and merely cosmetic in nature can often be treated with medicated make-up, over-the-counter skin care products, hygiene techniques, and small lifestyle changes. In addition, some skin conditions can be treated or improved with changes in diet. Some skin disorders cannot be prevented; genetic conditions and disorders that are brought on by other illnesses cannot be avoided. However, it is possible to prevent some skin disorders. Learning about proper skin care and skin disorder treatment can be very important for skin health. Some conditions require the attention of a doctor, while others can be safely addressed at home.
Continue to the next page to get tips on treating calluses - a foot condition almost everyone experiences at one time or another. Foot Injuries : Find out how to avoid unpleasant injuries to your feet, or at least reduce pain and prevent infection after they occur, with these simple suggestions. How to Care for Your Feet : Learn how to keep your feet - and yourself - healthy and happy with these tips on caring for your feet, including selecting the right shoes. For ladies that love to wear high heel footwear, the physics are immutable.
When a patient suffers a foot or lower leg injury they should see a podiatrist as soon as possible to receive the appropriate advice and treatment. The podiatrist will need to understand the cause of the injury, any previous injuries and the level of activity prior to the injury occurring. A comprehensive biomechanical assessment of the patient walking or running will then be carried out to outline any issues with foot/knee or hip alignment that may be causing or contributing to the condition. Podiatrists care for any skin and nail problem involving the feet. The skin may turn red, and start peeling.
Since plantar fascia gets tightened while one is asleep, the sudden movement causes stretching of the ligament as one takes the first few steps. While structural foot abnormalities such as high arches or fallen arches can make one more susceptible to plantar fasciitis, wearing old worn-out shoes can also cause stress to the plantar fascia. Those suffering from plantar fasciitis are also at an increased risk of developing heel spurs. Heel spurs, also known as osteophytes, are abnormal bony outgrowths that may develop along the edges of the heel bone. Heel spurs form when the plantar fascia starts pulling at the heel bone or gets torn due to excessive stress. If the heel spurs start impinging on any of the surrounding nerves or the tissues, one is likely to suffer from pain. Plantar fasciitis and heel spurs surely affect one's ability to move about freely. This is the best way to support the arch of the foot. Pain then sets in and you may need surgery.
Using Listerine for severe foot conditions can be wrong for example, for example, if you have cuts and wounds in case of toenail fungus, cracked heels, warts, corns and calluses, you must go for taking medical assistance to get relief from this painful and severe condition of feet. But some says feet skin gets green spots on feet while using cool mint Listerine. So it can be used confidently as it is reliable home remedy to treat feet problems. Plain cornstarch makes a great foot dusting powder.

All About Achilles Tendonitis
 Achilles tendinitis is a common condition that causes pain along the back of the leg near the heel. The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration. Simply defined, tendinitis is inflammation of a tendon. Inflammation is the body's natural response to injury or disease, and often causes swelling, pain, or irritation. There are two types of Achilles tendinitis, based upon which part of the tendon is inflamed. Noninsertional Achilles tendinitis, Noninsertional Achilles Tendinitis. In noninsertional In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may also calcify (harden). Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
Achilles tendinitis is a common condition that causes pain along the back of the leg near the heel. The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration. Simply defined, tendinitis is inflammation of a tendon. Inflammation is the body's natural response to injury or disease, and often causes swelling, pain, or irritation. There are two types of Achilles tendinitis, based upon which part of the tendon is inflamed. Noninsertional Achilles tendinitis, Noninsertional Achilles Tendinitis. In noninsertional In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may also calcify (harden). Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
Causes
Unusual use or overuse of the lower leg muscles and Achilles tendon is usually the cause of Achilles tendinitis. Repetitive jumping, kicking, and sprinting can lead to Achilles tendinitis in both recreational and competitive athletes. Runners, dancers, and athletes over age 65 are especially at risk. Sudden increases in training or competition can also inflame your Achilles tendon. For example, adding hills, stair-climbing, or sprinting to your running workout puts extra stress on your Achilles tendon. Improper technique during training can also strain the tendon. Intense running or jumping without stretching and strengthening your lower leg muscles can put you at risk regardless of your age or fitness level. Running on tight, exhausted, or fatigued calf muscles can put added stress on your Achilles tendon, as your tendon may not be ready to quickly start a workout after a period of inactivity. Direct blows or other injuries to the ankle, foot, or lower leg may pull your Achilles tendon too far and stretch the tissue. A hard contraction of the calf muscles, such as can happen when you push for the final sprint in a race, can strain the tendon. People whose feet roll inward, a condition called overpronation, are particularly at risk. Sometimes, shoes with too much heel cushioning put extra strain on the Achilles tendon.
Symptoms
If you have Achilles tendinitis or Achilles enthesopathy, you are likely to experience the following symptoms. Pain. You may notice aching, burning, or tearing pains at the back of your heel or above the ankle. The pain can range from mild to very severe and disabling. It is most noticeable in the following circumstances. After resting. Many people report that pain increases when they first get out of bed in the morning or after sitting for a period of time. After exercise. Pain may increase if you exercise or stand for a period of time. A lump. In some cases, a tender lump can develop at the site of the injured tendon (tendinosis). Bone spurs. When the injury occurs at the point where the tendon attaches to the foot, a bone spur may develop on the heel.
Diagnosis
The diagnosis is made via discussion with your doctor and physical examination. Typically, imaging studies are not needed to make the diagnosis. However, in some cases, an ultrasound is useful in looking for evidence of degenerative changes in the tendon and to rule out tendon rupture. An MRI can be used for similar purposes, as well. Your physician will determine whether or not further studies are necessary.
Nonsurgical Treatment
Most cases of Achilles tendonitis can be treated at home. Here's what to do. Stop doing the activity that led to the injury. Avoid putting stress on your legs and feet, and give your tendon plenty of time to fully recover. Use the RICE formula. Don't exercise for a few days, or try an exercise that doesn't stress your feet, such as swimming. If necessary, your doctor may recommend that you use crutches or wear a walking boot to keep weight off your foot. Apply an ice pack wrapped in a towel or a cold compress to your tendon for 15 minutes or more after you exercise or if you feel pain in the tendon. Use tape or an athletic wrap to keep swelling down and help support and immobilize the tendon. Lie down and raise your foot above the level of your heart, and if possible, try to sleep with your foot elevated. This will help keep the swelling to a minimum. Take anti-inflammatory medications. Pain relievers like ibuprofen can help ease pain and reduce swelling in the affected area. Stretch and exercise your ankles and calf muscles while you recover. Keeping your muscles, tendons, and ligaments strong and flexible will aid in your recovery and help you keep from reinjuring your Achilles tendon. A doctor or a physical therapist can help you come up with a good exercise program. Try a pair of prescription orthotic inserts for your shoes if your doctor thinks it will help. Sometimes orthotics can be helpful. Talk to your doctor or someone trained in fitting orthotics to find out if they might work for you. Achilles tendon surgery is rarely needed. It's usually only done if the tendon breaks, and then only as a last resort after other methods of therapy have been tried. Most cases of Achilles tendonitis will get better on their own with rest and minor treatment.

Surgical Treatment
Percutaneous Achilles Tendon Surgery. During this procedure the surgeon will make 3 to 4 incisions (approx. 2.5 cm long) on both sides of the Achilles tendon. Small forceps are used to free the tendon sheath (the soft tissue casing around your Achilles tendon) to make room for the surgeon to stitch/suture any tears. Skilled surgeons may perform a percutaneous achilles tendon surgery with ultrasound imaging techniques to allow for blink suturing with stab incisions made by a surgical suture needle. This procedure can be done in 3 different ways depending on the preference and experience of your surgeon. Instead of making several 2.5 cm incisions for this procedure, some surgeons will use guided imaging with an ultrasound to see the Achilles tendon tissue without having to open up your ankle. For this technique, they will use a surgical needle to repeatedly stab your Achilles tendon. These "stab incisions" will allow the surgeon to "blindly" suture your tendon without seeing the actual tissue. As another option - some surgeons will only make 1 to 3 incisions for smaller surgical implements to repair your tendon while relying on imaging ultrasound to see your damaged tissue. During either procedure the use of ultrasound imaging or endoscopic techniques requires a very skilled surgeon.
Prevention
You can take measures to reduce your risk of developing Achilles Tendinitis. This includes, Increasing your activity level gradually, choosing your shoes carefully, daily stretching and doing exercises to strengthen your calf muscles. As well, applying a small amount ZAX?s Original Heelspur Cream onto your Achilles tendon before and after exercise.
Heel Spur Symptoms
In case you have heel discomfort or this problem, arch supports are crucial. A contributing trigger of heel troubles is wearing shoes that won't adequately cushion the heel. In case your heel just isn't secured, every single time you action recorded on it you are injuring it. Over time, inflammation sets in and you'll have persistent heel ache. The bottom line is that if you looking how to get rid of plantar fasciitis you are going to need to rest and do stretches. I have a few resources areas that you can check out that offer valuable books and products, please visit natural remedies for plantar fasciitis for detailed information. Single-fraction patients are given a relatively larger dose in one treatment. In multiple-fraction radiation, patients get smaller doses, usually on consecutive work days. That means that patients, often older and not feeling well, must come repeatedly to the treatment center. Bekelman said a large clinical trial in 2005 concluded that the two regimens provide equal pain control with similar side effects. Some say patients are more likely to require a second round of treatment with single-fraction therapy, but Bekelman said evidence was mounting that the two forms of treatment are equal, even when it comes to retreatment. Pain that occurs in the bottom of the heel, typically plantar fasciitis, can make exercise and even just walking difficult. Several stretches can relieve foot pain in the bottom of the heel including the stair stretch, towel stretch, and standing calf stretch. Any questions about persistent foot pain, plantar fasciitis, or treatments for foot injuries should be directed to an individual's medical professional. Plantar fasciitis commonly causes stabbing pain in the hell when getting out of bed in the morning. Once your foot limbers up, the pain of plantar fasciitis is typically less severe, but may return after standing for longer periods or after getting up from a seated position. Physical therapy is used commonly to help rehabilitate patients with this condition to not only speed up recovery but also teach the patient how to properly exercise the plantar fascia if future events of this condition arise. Extracorporeal shock wave therapy, or ESWT, has emerged as a treatment option available for patients with plantar fasciitis ESWT delivers a focused shock waves to the heel. The healing response caused by the trauma causes the formation of blood vessels and an increase delivery of nutrients to the area thus stimulating a repair process to relieve the symptoms of plantar fasciitis. Plantar fasciitis subsides with conventional treatment in 94% of instances. Yet, in serious cases where heel pain is inciting regular walking then an injection with a mixture of corticosteroid and localized anaesthetic can be a good help. Following this injection, the patient is required to ease for a few days and normal activities can be resumed step by step. Pain can also occur during or after exercise or after standing for long periods of time. However, gradual onset of dull pain which turns into sharp pain as the day progresses is also common. It seemed my condition was very bad because I experienced all of these types of pain. There are various natural remedies for swelling. Something as fundamental as cinnamon, which may be acquired for your neighborhood grocery or drug keep, is really a excellent anti-inflammatory. Ginger root is in the course of herbs called "Cox inhibitors". Meaning they cease irritation naturally. Cinnamon is one for the weaker health supplements for irritation, but in a pinch a higher dosage could be useful. It will take a small time to mend this condition. Because you are strolling every day, you are regularly re-injuring the heel. In the event you proceed to use natural cures like Bromelain, systemic enzymes and Boswellin cream, ultimately the swelling will likely be settled entirely. The scenario is familiar to many – your alarm goes off and as you step out of bed to get ready for the day, you are met with stabbing foot pain! Can you relate to this? If so, you most likely have a foot condition called plantar fasciitis. Feet endure so much stress, and sometimes the only way they can tell us something is wrong is by crying out, literally. Marble pickup. Use your big toe and second toe to pick up marbles from the floor by curling your toes over the marbles—small stones will also work. With yor toes, deposit the marbles/stones into a different location. Repeat 10-15 times. The surgical treatment for treating this foot issue is carried out by partially releasing the plantar fascia to release the tension and alleviate the heel soreness. The heel bone spur that typically accompanies this foot condition will also be taken out. The surgery is frequently completed employing a neighborhood anesthetic and, barring complications, the indiv Plantar fasciitis can be acute, that is, as simple strain of the ligament but often is chronic, hanging on for months if not years. Why does that happen? The answer is poor foot mechanics, the foot sinking down too far alllowing the plantar fascia to overstretch with each step taken. I've had personal experience with Haflinger wool clogs. I wore them indoors and outdoors for years before they wore out. And even though they're all worn through in the uppers, I still wear them indoors. I have plantar fasciitis, and wide feet, and I found the clog is pleasantly roomy and their arch support is comparable to Birkenstock. When I'm having a flare-up, I wear my Haflingers as I putter around the house, summer or winter. They breathe in the summer and are cozy warm in the winter. I truly love them and recommend them for people looking for slippers for plantar fasciitis sufferers.
Plantar fasciitis subsides with conventional treatment in 94% of instances. Yet, in serious cases where heel pain is inciting regular walking then an injection with a mixture of corticosteroid and localized anaesthetic can be a good help. Following this injection, the patient is required to ease for a few days and normal activities can be resumed step by step. Pain can also occur during or after exercise or after standing for long periods of time. However, gradual onset of dull pain which turns into sharp pain as the day progresses is also common. It seemed my condition was very bad because I experienced all of these types of pain. There are various natural remedies for swelling. Something as fundamental as cinnamon, which may be acquired for your neighborhood grocery or drug keep, is really a excellent anti-inflammatory. Ginger root is in the course of herbs called "Cox inhibitors". Meaning they cease irritation naturally. Cinnamon is one for the weaker health supplements for irritation, but in a pinch a higher dosage could be useful. It will take a small time to mend this condition. Because you are strolling every day, you are regularly re-injuring the heel. In the event you proceed to use natural cures like Bromelain, systemic enzymes and Boswellin cream, ultimately the swelling will likely be settled entirely. The scenario is familiar to many – your alarm goes off and as you step out of bed to get ready for the day, you are met with stabbing foot pain! Can you relate to this? If so, you most likely have a foot condition called plantar fasciitis. Feet endure so much stress, and sometimes the only way they can tell us something is wrong is by crying out, literally. Marble pickup. Use your big toe and second toe to pick up marbles from the floor by curling your toes over the marbles—small stones will also work. With yor toes, deposit the marbles/stones into a different location. Repeat 10-15 times. The surgical treatment for treating this foot issue is carried out by partially releasing the plantar fascia to release the tension and alleviate the heel soreness. The heel bone spur that typically accompanies this foot condition will also be taken out. The surgery is frequently completed employing a neighborhood anesthetic and, barring complications, the indiv Plantar fasciitis can be acute, that is, as simple strain of the ligament but often is chronic, hanging on for months if not years. Why does that happen? The answer is poor foot mechanics, the foot sinking down too far alllowing the plantar fascia to overstretch with each step taken. I've had personal experience with Haflinger wool clogs. I wore them indoors and outdoors for years before they wore out. And even though they're all worn through in the uppers, I still wear them indoors. I have plantar fasciitis, and wide feet, and I found the clog is pleasantly roomy and their arch support is comparable to Birkenstock. When I'm having a flare-up, I wear my Haflingers as I putter around the house, summer or winter. They breathe in the summer and are cozy warm in the winter. I truly love them and recommend them for people looking for slippers for plantar fasciitis sufferers.
How To Treat Common Foot Problems Corns, Bunions, Ingrown Toenails And More
So in closing, give it another month, take a look at your shoes and if the pain continues, see a foot specialist, but before you consent to additional surgery, see if there are other options available to you. Dr. Richard Moy DPM, is a foot and ankle surgeon in Southern California who solves all types of foot and ankle problems. Dr. Moy performs more bunion surgeries than any other doctor worldwide! If you or someone you know is suffering from foot pain or bunions, you're a big step closer to the cure. If you have a bunion that is causing pain and discomfort, you may want to consider surgery. If this is the case, then you need to schedule an appointment with a foot surgeon. During your consultation, he will review your medical history and will determine whether or not your pain limits your everyday activities, if you have inflammation or stiffness of the big toe, and see if anti-inflammatories or other treatments can help. If no other options work, foot surgery may be your last option. Podiatrist suggests patients to go through a physical examination and perform X-ray evolution if required, perform trimming or padding of the lesions, surgery as required. If your loved one is not of an age that foot treatment is possible, then home remedies can be used to help alleviate pain. In most cases, elderly adults with bunion arthritis will benefit from daily foot massages, orthopedic shoes, and the use of massage therapy to ambulate the toes and ankles. By providing these services at home, you can help to alleviate pain but, again, the bunion arthritis will not be resolved. Failure to obtain pain relief from nonsteroidal anti-inflammatory drugs. Their effectiveness in controlling toe pain varies greatly from person to person.![]() Wearing inappropriate footwear leads to a damaging ailment known as a bunionette or tailor's bunion They are smaller than big toe bunions, but are essentially the same, just smaller and in a different location. They are the body's response to pressure, and serve to protect the feet from excess pressure and friction. Often this can cause pain and discomfort to the sufferer. This condition mainly affects women, especially those who wear fashionable and trendy footwear. Traditional open bunion surgery involves making a cut of 5cm on the outside of the foot and a smaller incision on the inside of the toe to release the tissues holding the toe. After the bunionectomy, the surgeon sutures the site and places sterile bandages on the area. Post operative care is necessary to be able to recover early. Initially, there will be swelling and pain on the operative site. The doctor will prescribe anti inflammatory medications to control the pain , swelling and redness that may occur. Support the foot without bearing weight on it or applying any pressure to be able to heal properly. A special shoe or a cast may be worn on the area after the bunionectomy as well. Constant follow up is needed to asses healing and any complications of the surgery. If your condition continues after a few months of plantar fasciitis treatment, your doctor may suggest injecting your heel with steroidal anti-inflammatory medications (corticosteroid). If you still have symptoms after the injection, you may need to wear a walking cast for 2-3 weeks or night splint when you sleep. In a few cases Usually, those who have bunions tend to take pain killers to get relief from the pain. However, such medicines should not be taken for a long time as they have adverse effects on the health. Hence, you can try out one or more of the following home remedies to reduce the pain.
Wearing inappropriate footwear leads to a damaging ailment known as a bunionette or tailor's bunion They are smaller than big toe bunions, but are essentially the same, just smaller and in a different location. They are the body's response to pressure, and serve to protect the feet from excess pressure and friction. Often this can cause pain and discomfort to the sufferer. This condition mainly affects women, especially those who wear fashionable and trendy footwear. Traditional open bunion surgery involves making a cut of 5cm on the outside of the foot and a smaller incision on the inside of the toe to release the tissues holding the toe. After the bunionectomy, the surgeon sutures the site and places sterile bandages on the area. Post operative care is necessary to be able to recover early. Initially, there will be swelling and pain on the operative site. The doctor will prescribe anti inflammatory medications to control the pain , swelling and redness that may occur. Support the foot without bearing weight on it or applying any pressure to be able to heal properly. A special shoe or a cast may be worn on the area after the bunionectomy as well. Constant follow up is needed to asses healing and any complications of the surgery. If your condition continues after a few months of plantar fasciitis treatment, your doctor may suggest injecting your heel with steroidal anti-inflammatory medications (corticosteroid). If you still have symptoms after the injection, you may need to wear a walking cast for 2-3 weeks or night splint when you sleep. In a few cases Usually, those who have bunions tend to take pain killers to get relief from the pain. However, such medicines should not be taken for a long time as they have adverse effects on the health. Hence, you can try out one or more of the following home remedies to reduce the pain.